Photodynamic (PDT) and Sonodynamic Therapies (SDT)
For the treatment for cancer using light and ultrasound.

Background
Photodynamic therapy (PDT) is a form of phototherapy using nontoxic light-sensitive drugs (called photosensitizer or sensitizer for short) that are exposed selectively to light whereupon they cause targeted malignant and other diseased cells to die off.
Similarly, sonodynamic therapy (SDT) makes use of therapeutic ultrasound instead of light to activate sensitizer compounds allowing a much deeper penetration to target cancer cells in the body.
Photodynamic therapy (PDT) and sonodynamic therapy (SDT) may be used individually or in combination depending on the disease, stage of development, various individual circumstances or other factors determined by the physician and the patient. When PDT and SDT are both used for treatment the therapy is sometimes referred to as sonophotodynamic therapy (SPDT).
- Sono = (ultra)sound
- Photo = light
PDT and SDT technology have been developing all over the world for a long time but some parts are relatively new and the therapy is still evolving. Newer sensitizers are becoming available to target cancer cells in somewhat different ways.
Therapy Overview
1. Administration
A light-sensitive and ultrasound-sensitive drug (called photosensitizer) is administered intravenously, orally or topically.
Sensitizers commonly have a chlorophyll or porphyrin ring structure which provides sensitivity to light.
Sensitizers have the characteristic of being absorbed preferentially by cancer cells and diseased cells rather than by normal healthy cells.
2. Activation
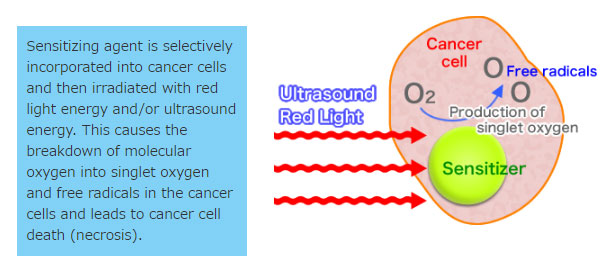
- Photosensitizers are sensitive to specific wavelengths of light and ultrasonic waves which are absorbed by the sensitizer during the PDT and SDT treatment. In the activation process, this light and ultrasound energy break up molecular oxygen into singlet oxygen and free radicals, thereby destroying the cancer cells.
- Photosensitizers are non-toxic and have minimal side effects.
- Treatment should be continued as long as necessary as long as the disease is present, in combination with a variety of other modalities such as GcMAF macrophage activating therapy.
Mechanism of Cancer Cell Death (Necrosis)
Benefits of PDT and SDT Therapies
- Sensitizers are non-toxic and safe to use repeatedly as there is no total dosage limitation
- Treatment is targeted primarily at tumors with minimal effect on healthy tissue.
- PDT and SDT therapies does not suppress immune functions. In fact, quite the opposite is true. PDT and SDT therapies are a perfect complement to immuno-therapies such as GcMAF and Hyper T/NK therapy which enhance immune activity.
- Vaccine-like response from immunogenic cancer cell necrosis and cancer-immune response.
Treatment Factors and Limitations
- The depth of light penetration limits the depth of activation.
- Sufficient light needs to reach the tumor in order to activate the breakdown of oxygen which kills the cancer cell.
- The limited depth of penetration of light is overcome by the use of ultrasonic waves which activate the drug at greater depths.
- Ultrasound is commonly used in medicine as it can safely penetrate deep into body tissues
- The therapy which activates a sensitizer by ultrasound instead of light is called Sonodynamic Therapy (SDT).
Sonodynamic Therapy (SDT)
- Ultrasound was first found to enhance the effect of chemotherapy drugs in 1976.
- It was subsequently discovered that several photosensitizers are also activated by ultrasound and referred to as a “sono-sensitizer”.
- Ultrasound creates a mechanical effect on the sono-sensitizer which causes:
- Production of oxygen-free radicals
- Sonoporation (physical destabilization of cell membranes)
- – Cavitation
- Sonodynamic therapy allows deep tumors to be treated and has the advantage of being non-invasive and targeted due to the selective sensitizer uptake by the cancer cells.
What Are the Benefits of Sonodynamic Therapy?
Sonodynamic therapy––a review of the synergistic effects of drugs and ultrasound (2004). I Rosenthal, J Sostaric, P Riesz. Ultrasonics Sonochemistry.
Abstract
The abstract reviews sonodynamic therapy, the ultrasound-dependent enhancement of cytotoxic activities of certain compounds (sonosensitizers) in studies with cells in vitro and in tumor bearing animals. The attractive features of this modality for cancer treatment stem from the ability to focus ultrasonic energy on malignancy sites buried deep in the tissue and to locally activate a preloaded sonosensitizer. Possible mechanisms of sonodynamic therapy include the generation of sonosensitizer-derived radicals which initiate chain peroxidation of membrane lipids via peroxyl and/or alkoxyl radicals, the physical destabilization of cell membranes by the sonosensitizer, thereby rendering the cell more susceptible to shear forces or ultrasound-enhanced drug transport across cell membranes (sonoporation). Evidence against the role of singlet oxygen in sonodynamic therapy is discussed. The mechanism of sonodynamic therapy is probably not governed by a universal mechanism, but may be influenced by multiple factors including the nature of the biological model, the sonosensitizer and ultrasonic parameters. The current review emphasizes the effect of ultrasound-induced free radicals in sonodynamic therapy.
Safety of Sensitizers
- Safety studies using a Zebrafish Model (a widely used safety test) have shown an excellent safety profile even at maximum soluble concentrations.
- Advice is given to avoid bright sunlight during treatment but no cases of skin sensitivity were noted.
Tumor Hypoxia and Ozone Therapy
- Tumors are low in oxygen (hypoxic).
- Poor blood oxygenation can reduce the effectiveness of chemotherapy, radiation therapy as well as of photodynamic and sonodynamic therapies.
- Ozone autochemotherapy (Ozone Therapy) is performed prior to light and ultrasound activation to increase tumor oxygenation.
- Research has demonstrated increased tumor oxygenation following ozone administration.
Treatments Used in Conjunction with Photodynamic and Sonodynamic Therapies
GcMAF Therapy

Hyperbaric Oxygen Therapy

Hyperthermia

Ozone Therapy
Treatment process
Photodynamic Therapy (PDT) and Sonodynamic Therapy (SDT):
1 cycle (2 weeks), 6 treatments
Depending on the patient, the treatment includes either ozone autohemotherapy (ozone therapy) or use of a hyperbaric air chamber to increase the oxygen level in the cells.
- 3 days of treatment are required per week.
- Application of light and/or ultrasound is on 3 days per week.
- The exact treatment protocol varies slightly between patients and is customized by the physician to the individual patient.













